On July 13th, the Centers for Medicare & Medicaid Services (CMS) issued proposals to update the Medicare physician fee schedule payments and policies for 2024 – available HERE. Beyond payment policies, the rule also includes proposals to implement changes to the quality payment program (QPP) and a proposed indefinite delay to the Appropriate Use Criteria /Clinical Data Support (AUC / CDS).
2024 Conversion Factor
- Proposed Medicare Fee Schedule CF: $32.74
- Decrease of -$1.15 from 2023 CF of $33.89
- Proposed Anesthesia CF: $20.43
- Decrease of -$.69 from 2023 CF of $21.12

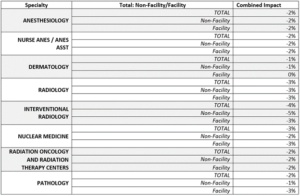
*Full specialty impact table is available within the proposed rule – Be aware that different billing arrangements may influence the final outcomes of CMS’s estimated impacts.
PAYGO Cuts Delayed:
As a reminder, the Omnibus legislation that was passed at the end of the 2023 year, prevents a statutory Pay-As-You-Go reduction from taking effect until at least 2025. This ‘PAYGO’ cut was the result of spending included in the American Rescue Plan, which triggered a budget control mechanism to apply automatic reductions in order to achieve budget neutrality.
From the American Hospital Association in December 2022:
The House and Senate Appropriations Committees last night released the fiscal year 2023 Omnibus Appropriations legislation that would fund the government through Sept. 30, 2023. The bipartisan bill includes various provisions beneficial to hospitals and health systems.
The legislation would:
- Prevent the 4% Statutory Pay-As-You-Go (PAYGO) sequester for two years;
- Reduce the physician fee schedule cut from 4.5% to 2% for 2023 and approximately 3% for 2024
Appropriate Use Criteria/Clinical Decision Support
Due to challenges during the testing phase of the program, CMS has proposed an indefinite pause on the Appropriate Use Criteria (AUC) also known as the Clinical Decision Support program. This would effectively end the current educational and testing period for the program and allow CMS to reevaluate the AUC as a whole. There is no timeline on when or if this program would be reintroduced.
The CMS had this to say on the AUC program in this year’s proposed rule:
“Taken together and, in particular, due to the inability of the Medicare claims processing system to automate claims processing edits that ensure only claims subject to the AUC program requirements as prescribed in section 1834(q) of the Act will be processed as such, returned or denied accordingly, we believe the inherent risks in terms of data integrity and accuracy, beneficiary access, and potential beneficiary financial liability for advanced diagnostic imaging services render the AUC program impracticable, and have led us to our proposal to pause efforts to implement the AUC program for reevaluation and rescind current regulations. Working within the parameters prescribed under section 1834(q) of the Act, we have not identified any practical way to move the AUC program forward beyond the educational and operations testing period. Further, without a way forward to fully implement the AUC program, we believe there is no utility in continuing the educational and operations testing period. We will continue efforts to identify a workable implementation approach and will propose to adopt any such approach through subsequent rulemaking. We note, and discuss further below in this section of the proposed rule, that clinical decision support tools can be beneficial in assisting with clinical decision making and we encourage continued use of clinical decision support in a manner that best serves and assists clinicians.”
Changes to Evaluation and Management Visits
CMS has proposed applying a new add-on HCPCS code, G2211, for E/M visits. This new code would capture additional resources being utilized for primary care and specialties who treat a single, serious condition or a complex condition with a consistency and continuity over an extended time frame. The operation of the code has been revamped since its first proposal in 2020 when Congress put a pause on the code until at least 2024. If confirmed, the G2211 code would have redistributive impacts for all other 2024 payments but still have less of an impact as originally proposed in 2020.
In additional CMS looks to maintain the split/shared E/M billing rules. They have proposed the delay of altering the definition of “substantive portion” until 2025. Under the proposal, clinicians who furnish split (or shared) visits will continue to have a choice of history, physical exam, or medical decision making, or more than half of the total practitioner time spent to define the substantive portion, instead of using total time to determine the substantive portion, until CY 2025.
Quality Payment Program (QPP/MIPS)
CMS has proposed several changes to the QPP’s Merit-based Incentive Program System or MIPS program for the 2024 performance year.
Here are some of the highlighted proposed changes:
- An increase to the MIPS Performance threshold of 7 points making the penalty threshold 82 points.
- Data completeness threshold for Quality measures would increase by 5% making the new threshold 75%.
- CMS has proposed the removal of the following three Radiology- related measures:
- MIPS 147: Nuclear Medicine: Correlation with Existing Imaging Studies for All Patients Undergoing Bone Scintigraphy
- MIPS 324: Cardiac Stress Imaging Not Meeting Appropriate Use Criteria: Testing in Asymptomatic, Low-Risk Patients
- MIPS 436: Radiation Consideration for Adult CT: Utilization of Dose Lowering Techniques
As always, ADVOCATE will keep you up to date on this and all issues impacting medical groups as they become available.
Advocate’s Regulatory Team