By Jennifer Bash, RHIA, CIRCC, RCCIR, CPC, RCC, CANPC
Director of Coding Education
In a world of rapidly growing technology, Artificial Intelligence (AI) is the new buzz word. But how can you stay informed, educated, and make the right choices for your radiology practice?
The Data Science Institute of the American College of Radiology has received positive feedback from multiple healthcare settings and confirmed that AI tools “significantly contribute to clinical efficacy and efficiency when effectively integrated.” In a recent blog they go on to say, “larger practices currently have a higher adoption rate, AI algorithms have the potential to bridge the gap in areas with a shortage of radiologists, thereby extending their benefits across a wider range of healthcare environments.” So what does this mean for your practice?
History of New Technology Adoption in Radiology
Over the last few decades, the adoption of new technologies in healthcare has come a long way. Advancements that were once considered experimental are now the gold standard of medical practice. This is no different in radiology, however, progress did not come easy. The adoption of new technologies, both from a clinical standpoint and coding and reimbursement, often moved at a slow pace. Because of patient care, the acceptance of new technologies in the clinical space moves a little more quickly, whereas coding and reimbursement often lags behind clinical adoption. As a result, practices can be hesitant to invest in new technology without knowing if or when a CPT code will be developed, and if they will see a return on their investment.
To illustrate this point, let’s consider a couple of examples. First, digital breast tomosynthesis is now widely considered the gold standard in baseline breast imaging. While tomosynthesis was originally developed in the 1970s, it was not FDA-approved until 2011—over 40 years later! A Category I CPT code was released in 2015, and still today Medicare has their own coding and reimbursement structure for their beneficiaries for this procedure. Another example is ultrasound elastography, which was developed in 1991 and FDA-approved in 2013. Soon after, it received a Category III code in 2014. However, a Category I code, which is assigned a reimbursement rate, was not released until 2019—a 28-year process.
CPT Code Development Process
The exciting news is that we are beginning to see this process move a little quicker as AI technologies are rapidly being developed. The AMA owns and authorizes CPT codes, and new technologies are constantly under review for code assignment. There is even a new AI classification system within the CPT manual to support all the new codes.
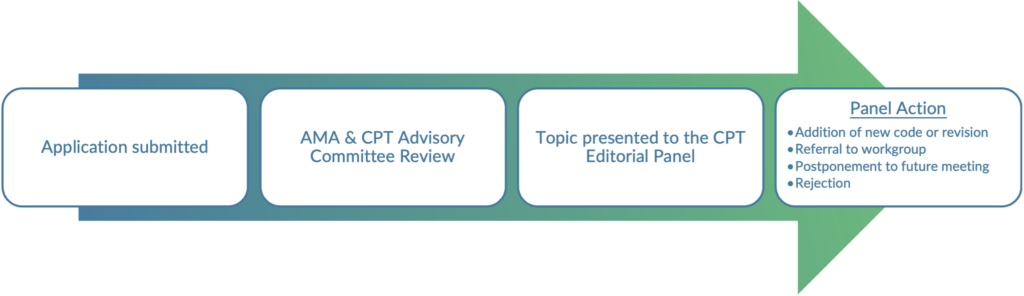
To better understand how technology moves into the code development process, it is important to know the basics of CPT code development. CPT codes offer providers a uniform language for coding services for reporting and administrative purposes, both in the RCM and clinical aspects. Development of the code set is led by the CPT Editorial panel with input from the CPT Advisory Committee and the development process is intended to ensure that “clinically valid codes are issued, updated, and maintained on a regular basis to accurately reflect current clinical practice and innovation in medicine.”
CPT codes are broken into three categories: Category I, II, and III. Category I codes are established codes in the CPT manual and are generally assigned a reimbursement value. Category II codes are alphanumeric tracking codes used for performance measurement like the Quality Payment Program. Using Category II codes is optional and not required for correct coding. Category III codes are temporary, alphanumeric codes for new and developing technology, procedures, and services. They were created for data collection, assessment, and in some instances, payment of new services and procedures that currently don’t meet the criteria for a Category I code. There are different criteria required for obtaining Category I and Category III status.
The general application process is illustrated below:
AI Emergence in Radiology
How does AI in radiology fit into this current landscape? More and more radiology practices are utilizing some type of AI. Some of this AI adoption in radiology falls outside of the clinical aspect with AI tools largely addressing a practice’s administrative and business needs. These may include tools for enhancing radiology dictation and reporting and a variety of business management applications.
From a clinical standpoint, AI is exploding. The future of patient outcomes related to some of these applications is very exciting. However, there are currently over 650 radiology-specific AI applications that are FDA cleared and less than 20 have established CPT codes. All but one of those are Category III codes, which often are not reimbursed. The only application that obtained Category I status as of this year is Coronary FFR-CT, which we will highlight in the case study below.
Case Study
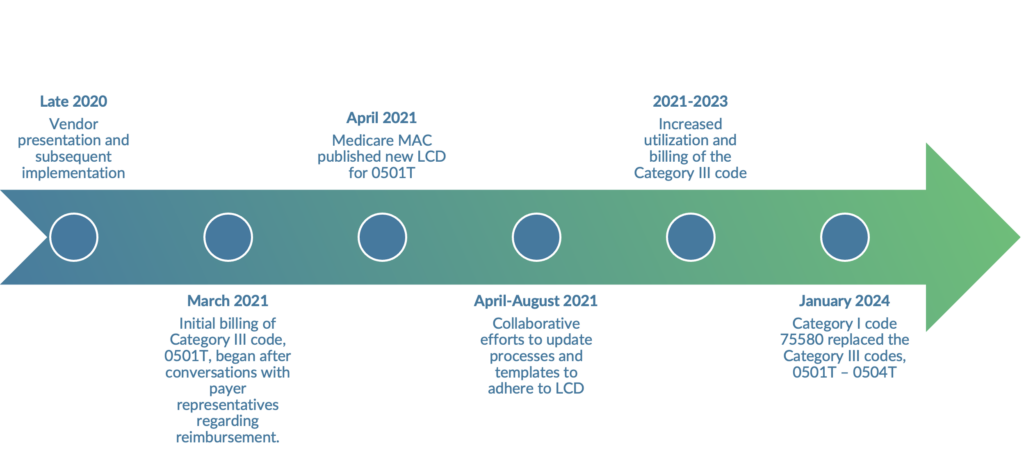
A radiology practice and ADVOCATE client began the process of reviewing a new AI application, Coronary Fractional Flow Reserve (FFR-CT) in 2020. FFR-CT uses a tool to analyze data from a CTA to generate a 3D model of the coronary arteries to more accurately identify blockages.
The timeline below demonstrates the pivotal moments for this client. Once the initial billings for FFR-CT began in 2021, the practice started receiving some reimbursement, but many payers still denied claims as experimental. Vendor assistance and a hospital stipend on denied claims provided additional financial assistance for the practice. Throughout 2022 there was a significant decrease in denials due to noncoverage, and reimbursement ramped up. Between 2021 and 2023 the practice experienced a 235% increase in collections for the procedure and this was WITHOUT a Category I CPT code. This is extremely encouraging and may signal that reimbursement for some of these AI applications could accelerate at an unprecedented pace.
This practice’s success was achieved through a collaborative effort involving the radiology practice, payers, and billing staff.
Key Takeaways & Tips for Adopting New Technologies
- When looking to invest in new technology, practices should consider the intended use and how it will be integrated into the existing workflow.
- Research into market demand and referrer education can mitigate potential losses
- Strong communication with hospitals is imperative.
- Strong payer relationships will enable better reimbursement feedback in advance.
- Medicare billing guidelines can be slow to incorporate the realities of new technologies. Code development and subsequent reimbursement can substantially lag technological development, but we are seeing some encouraging signs in the industry that the lag with AI applications may be reduced.
References:
https://www.ama-assn.org/practice-management/cpt/cpt-overview-and-code-approval
https://www.ama-assn.org/about/cpt-editorial-panel/cpt-code-process